Psychedelics And Chronic Pain: What Do We Know
You can be forgiven if psychedelics and chronic pain aren’t two things you think of as being related. Historically, psychedelic drugs like psilocybin (the psychoactive ingredient in “magic mushrooms”), LSD, DMT, and Mescaline have been associated with vivid and deeply introspective, kaleidoscopic “trips”, characterized by realizations of universal interconnectedness and increased empathy for all living things.
Of course, psychedelics have also been the subject of misguided, prejudiced propaganda warning users of the dangers of experimentation with these physiologically harmless, boundary dissolving compounds, which has ultimately plagued their reputation with falsehoods.
Finally, after half a century of an utterly irresponsible ban on psychedelic science, research investigating the therapeutic potential of these “mystical experience” inducing drugs has been resurrected by some brave and interested scientists. In recent years, researchers at universities all over the world have been demonstrating how psychedelics, in particular psilocybin, can be used in conjunction with psychotherapy to improve mental health conditions.
Studies conducted at Johns Hopkins University, New York University, Imperial College London, King’s College London, and many more, have shown that psychedelics when administered in a safely controlled environment by specially trained medical professionals, can be a profoundly curative treatment for anxiety, depression, post-traumatic stress disorder, and substance use disorders.
Now, based on anecdotal reports and preliminary evidence from case series, a growing number of researchers are investigating whether psychedelics could treat a variety of chronic pain conditions, and so far, the results have been encouraging.
Table of Contents
Previous Research Using Psychedelics To Treat Pain
Psychedelic research has largely focused on the ability of these fascinating compounds to effectively treat mental health conditions. The bulk of evidence in support of psychedelics as a potential treatment for chronic pain stems from case series and anecdotal reports, with very few clinical trials explicitly exploring their analgesic power ever having been conducted.
That said, the little evidence that does exist, going as far back as 1964, is undoubtedly suggestive of profound pain-relieving potential in a variety of chronic pain conditions. These include cancer-related pain, phantom limb pain, cluster headaches, and migraine.
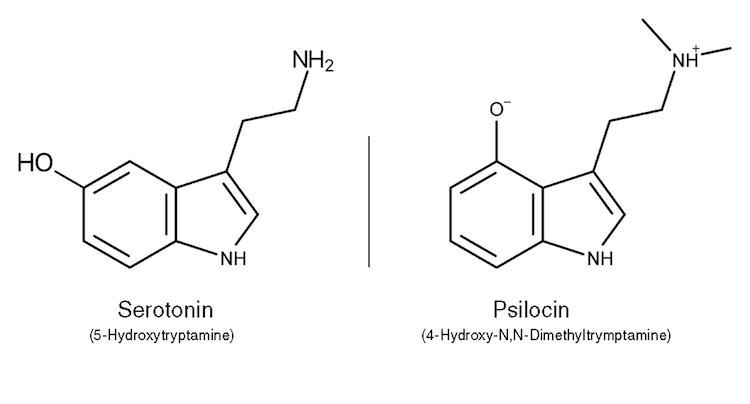
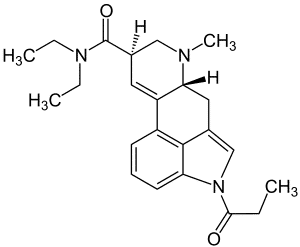
Classic psychedelic drugs share an ability to increase the activity of serotonin pathways involved in the processing and modulation of pain. In addition, their subjective effects are very similar, particularly in the case of LSD and psilocybin. As a consequence, there is considerable crossover between the therapeutic indices of classic psychedelics.
For these reasons, researchers have been prompted to speculate regarding their analgesic properties.
LSD and cancer-related pain
In 1964, Austrian-born pain physician and anesthesiologist, Dr. Eric Kast, conducted a study in which he compared LSD’s analgesic effects with two opioids — meperidine, and hydromorphone. 50 “gravely ill” participants participated in this study, the majority of whom were suffering from cancer and associated chronic pain.
Participants were first administered the opioid medications, before receiving 100 micrograms of LSD — a hefty dose sufficient to initiate a strong psychedelic experience in most people. According to Kast, LSD significantly outperformed the two opioids, producing profoundly analgesic effects that lasted up to 3 weeks in some participants.
In addition to pain relief, Kast reported that patients were more accepting of their diagnoses after their LSD experience. Patients who had terminal diagnoses were seemingly less perturbed by existential despair and began talking openly and fearlessly about their inevitable passing.
Interestingly, their more accepting and open-minded approach to illness outlasted the analgesic effects of LSD. Patients would regularly pass a casual comment on the horrific nature of their specific illness, before remarking on the beauty or pleasantness of an arising sensation.
After this publication, just two additional studies measured LSD’s ability to relieve pain in cancer patients. A study authored by renowned psychedelic researchers Walter Pahnke, Albert Kurland, Louis Goodman, and Bill Richards, investigating the effects of LSD-assisted psychotherapy in a cohort of terminally ill cancer patients, found that it significantly improved their pain.
Similarly, 4 years later, founder of transpersonal psychology and holotropic breathwork, and author of over 20 books on psychedelics and consciousness, Czech psychiatrist Dr. Stanislav Grof, led another investigation into LSD-assisted psychotherapy’s effects also in terminally ill cancer patients. In this study, the authors reported that LSD reduced chronic pain severity, preoccupation with chronic pain, and physical suffering associated with cancer.
Psilocybin and phantom limb pain
A recent case report suggests that psilocybin may be an effective treatment for phantom limb pain, a chronic pain condition affecting 8 out of 10 amputees in which ongoing painful sensations are felt to be coming from a part of the body that is no longer there.
Phantom limb pain experts believe that the ongoing pain is due to miscommunication between the brain and the spinal cord caused by the fact that nerve connections from the peripheral nervous system to the brain remain in place, even after the amputated limb has been removed.
A variety of pharmacotherapies are available for phantom limb pain patients, including Nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, antidepressants, anticonvulsants, beta-blockers, and muscle relaxers, however, these medications have provided little to no relief in most patients. Alternatively, patients can opt for treatments that send electrical impulses directly into the nervous system, including Neurostimulation, Spinal cord stimulation, and Transcutaneous Electrical Nerve Stimulation (TENS).
Again, in most cases, these treatments provide marginal, transient relief, and in some patients no relief at all.
Perhaps the most efficacious treatment for phantom limb pain is a neurorehabilitation technique developed by Indian-American neuroscientist Dr. Vilayanur Subramanian Ramachandran called mirror visual feedback (MVF). The central premise of MVF is essentially to trick the mind into seeing two limbs when, in actuality, there is just one, and to facilitate attunement of the part of the brain that is in a state of dissonance.
In 2018, UC San Diego researchers, Dr. Ramachandran among them, explained the fascinating story of award-winning scientist Dr. Albert Lin, who, after a tragic vehicular accident, was required to have one of his legs amputated just below the knee. Lin suffered from excruciating phantom limb pains several times a day in the aftermath of his surgery. After experiencing little to no relief using opioids, the anticonvulsant medication Pregabalin, or a combination of medicinal cannabis and MVF, he was forced to experiment with alternative options.
Lin turned to psilocybin-containing mushrooms as a last resort. Amazingly, a single dose of psilocybin mushrooms initiated powerful analgesic effects lasting 3 hours. Lin then experimented with a combination of psilocybin mushrooms and MVF and reported a 50% pain reduction lasting 3 weeks.
This combination therapy ultimately helped to completely resolve Lin’s phantom limb pain.
“When combined with Mirror Visual Feedback therapy – even though the intensity of pain was not significantly different,” the authors write, “the subsequent reduction of pain persisted for weeks and months following the procedure.” They go on, “Apparently, the combination of the mirror and the psilocybin synergize powerfully to produce a striking and long-term reduction of pain after just 3 “doses” of the combination.”
The researchers hypothesized that psilocybin’s activation of the 5-HT2A receptor may enhance communication between the visual and somatosensory cortex, and in so doing, streamline the effects of MVF. Psilocybin-induced cross-modal functional connection and neuroplasticity via 5-HT2A activation may make the brain more receptive to MVF, producing significant pain reductions or bringing a stop to pain altogether.
Psychedelics, cluster headache, and migraine
Conventional treatments for cluster headache, a particularly treatment-resistant chronic pain condition, largely fail to alleviate pain in sufferers. Unfortunately, they provide marginal relief in most cluster headache patients and none at all in many. However, several interesting case series suggest that psychedelic medicines could be an effective treatment option for patients in the future.
In 2006, a team of researchers conducted interviews with 53 people who had self-medicated with psilocybin or LSD to relieve cluster headaches. Here, it was uncovered that both psychedelics were highly effective abortive treatments, rapidly terminated cluster periods in over 50% of participants, and extended remissions periods in the vast majority of users.
“No other medication, to our knowledge,” Dr. Andrew Sewell and his co-authors, psychiatry professors Dr. John Halpern and Dr. Harrison pope Jr, report, “has been reported to terminate a cluster period … a single dose of LSD was described as sufficient to induce remission of a cluster period, and psilocybin rarely required more than three doses.”
A 2015 survey found similarly impressive results. It sought to further understand cluster headache patients’ experience self-medicating with a variety of different drug types, including psilocybin and LSD. Again, respondents reported that psilocybin was an effective abortive treatment, and was deemed highly effective as a prophylactic.
According to the study’s authors, who were members of the non-profit organization Clusterbusters, Inc., psilocybin and LSD provided over 70% of respondents with at least moderate protection from attacks. Furthermore, LSD and psilocybin prevented the onset of cluster headache in 40% of users, which is considerably greater than the protection provided by conventional medications.
Interestingly, the non-hallucinogenic LSD derivative 2-bromo-lysergic-acid-diethylamide, or BOL-148, has also produced profoundly positive outcomes in cluster headache patients. This opens up the possibility that the apparent efficacy of BOL-148, and perhaps all psychedelics, to treat pain, may have little to do with their ability to initiate psychedelic effects.
Regarding the ability of psychedelics to treat migraine pain, a qualitative analysis of online forum data found that psilocybin and LSD were effective for both prophylactic and acute treatment of migraines — reducing migraine frequency and pain intensity.
The first and only placebo-controlled trial investigating the ability of psilocybin to treat migraine found that it was significantly more effective than placebo, producing substantial reductions in migraine frequency and pain severity.
LSD decreases pain perception
To explore the analgesic effects of LSD, as demonstrated By Dr, Kast in the 1960s, Dr. Johannes Ramaekers of Maastricht University led a study in which 24 healthy volunteers were administered a Cold Pressor Test 90 mins and 5 hours after they had been given variable sub-hallucinogenic doses of LSD.
A single 20 microgram dose of LSD was found to significantly increase the amount of time that participants could tolerate exposure to cold water, and decreased their subjective levels of experienced pain and unpleasantness. This strong effect, comparable to some opioids currently being used to treat pain conditions, was surprising considering the relatively small dose of LSD that participants received.
Although results were promising, it’s important that they can be generalized to patient populations.
The study’s authors hypothesized that 5-HT2A and 5-HT1A serotonin receptors may play a role in LSD’s analgesic effects due to their location at serotonergic descending pathways from the raphe nucleus to the spinal cord involved in the processing of pain. Stimulation of these descending pathways influences the signaling of pain in the body, which is potentially why volunteers were more tolerant of the cold water.
Ramaekers is now working on a follow-up study that intends to replicate these findings, but this time in a cohort of patients suffering from fibromyalgia — an intractable condition that causes pain all over the body.
Co-authors of this study, Dr. Kim Kuypers of Maastricht University and Dr. Matthias Liechti of the University of Basel, are working in cooperation with MindMed, a leading psychedelic medicine company based in New York, to continue this fascinating investigation into LSD’s pain-relieving qualities.
Self-medication for chronic pain
A team of scientists from Imperial College’s Center for Psychedelic Research, of which leading psychedelic researcher Dr. Robin Carhart-Harris was a part, recently conducted semi-structured interviews with 11 people using psychedelics to treat their chronic pain.
In this study, chronic pain was associated with mixed pain conditions, including traumatic injury (e.g., whiplash), congenital condition (e.g., Femoroacetabular impingement), connective tissue condition (e.g., Ehlers-Danlos syndrome), chronic back pain, fibromyalgia syndrome, autoimmune disorders (e.g., Hashimoto’s disease).
Study participants had been suffering from chronic pain for between 2 and 25 years. All 11 interviewees had tried multiple pharmacological treatments, with three pursuing more invasive treatment options in radiofrequency ablation and surgery.
The psychedelic substances that were reportedly used for self-medication in this cohort of interviewees included psilocybin, LSD, DMT, and ayahuasca. The vast majority of participants reported the following positive effects:
- Lasting pain reduction
- Positive reframing of their relationship with pain
- Improved pain management
- Increased pain acceptance
- Increased control over pain
- Improved physical functioning
- Complete or partial analgesia during the psychedelic experience
- Lasting increases in positive embodiment and interoception
- Improvements in general well being
One interviewee who had used psilocybin-containing mushrooms to treat their pain declared:
“Every time I’ve done (mushrooms), it’s always reminded me that there’s a light at the end of the tunnel, that (the pain) might suck, but it’s not that bad. It’s totally manageable, I can be happy while all of this is going on.”
Another reported that DMT had a profound effect on their chronic back pain:
“My back was starting to feel like my other muscles, which is a huge difference for me…That’s like when I’m on DMT—it feels normal, which is such a foreign word to my mouth to just feel normal.”
Similarly, those who self-medicated with LSD also experienced profound relief:
“Every time that I have taken LSD, I have experienced relief the next day. Every single time… it helps with my state of mind the following days, but the pain specifically, I feel it always. I always get some relief. Always.”
Most interviewees were surprised and even shocked at the profound analgesic effects of their chosen psychedelic. The authors reliably identified two specific processes that may be particularly important for self-medicating chronic pain; Positive Reframing of one’s relationships to their pain, and somatic presence, which they describe as a kind of mindfulness of the body.
Importantly, all interviewees reported that they used psychedelics in conjunction with introspective practices including breathwork, mindfulness, and meditation, movement practices such as Yoga and Qi Gong, and integrative practices such as art and journaling.
The authors emphasized that data gathered from the interviewees would be used to inform the design of a future trial investigating the effects of psychedelics on chronic pain from fibromyalgia.
Growing Interest in Psychedelics To Treat Chronic Pain
With so many psychedelic medicine companies and research institutions looking at the potential of psychedelics to treat psychiatric disorders, newcomers to the psychedelic space are focusing their attention on the contribution psychedelics could make to the treatment of chronic pain conditions
A prime example of this are Tryp Therapeutics who have teamed up with Robin Carhart-Harris and specialist researchers from the University of Wisconsin-Madison and the University of Michigan to investigate psilocybin’s potential as a treatment for fibromyalgia, phantom limb pain, and complex regional pain syndrome. In particular, efficacy rates for existing fibromyalgia medications, Lyrica, Cymbalta, and Savella, are poor, with up to 30% of patients becoming addicted and 90% discontinuing therapy within a year.
Tryp plan to administer psilocybin-assisted psychotherapy in conjunction with preparatory and integrative psychotherapy sessions. However, the type of psychotherapy delivered will vary depending on the pain disorder being treated due to patients’ unique relationships with their specific pain disorder.
As a further matter, many psychedelic guides haven’t interacted with the pain patient population. It is vitally important to make sure that a patient’s autonomy is respected, and that they receive the assistance they need, when they need it, in both preparatory and integrative therapy sessions — this will be essential to ensure that they are adequately set up for success.
Tryp also intend to monitor biomarkers such as heart rate and blood pressure, and fMRI and EEGs will be carried out to get a more comprehensive understanding of neurological activity.
The California-based start-up also have plans to conduct research using their very own proprietary version of psilocybin, Tryp-8803, which may include mechanisms to terminate the psychedelic experience should a difficult trip compromise therapeutic progress. They are also exploring the possibility of employing a novel route of administration.
TRYP CEO Greg McKee believes that psilocybin’s ability to promote neural plasticity could help to disrupt learned neural patterns that are inconducive to healing and recovery.
MindMed recently announced that they will be conducting a series of studies using psychedelics to treat chronic pain. According to their official website, ‘Project Angie’ will explore two primary clinical indications for the treatment of pain.
Researchers at Yale University will soon be conducting a trial investigating psilocybin’s potential to treat cluster headaches, a pain condition currently affecting 300,000 people in the US.
University of California San Diego recently announced an upcoming placebo-controlled trial that will study the effects of psilocybin in patients with phantom limb pain. These researchers are also expected to publish a case series analyzing anecdotal reports of success that people have had self-medicating their chronic pain using psilocybin.
Finally, researchers at the University of California San Francisco are preparing a trial to explore the analgesic effects of psilocybin in patients with chronic low back pain.
Psychedelics and Chronic Pain: Here’s What We Know
One of the central tenets of pain medicine today is neuromodulation, a technology that acts directly on nerves through targeted delivery of magnetic/electrical stimulation or chemical agents. Neuromodulation changes the way neurons fire and, as a result, modulates how people perceive pain.
Up until recently, very few people had explored whether psychedelics could profoundly modulate the nervous system. Further investigation in this area may lead to a more comprehensive understanding of mechanisms of action, lead to a better understanding of how to modulate pain, and ultimately improve patients’ quality of life.
Evidence from uncontrolled case series for relieving pain associated with a variety of chronic pain conditions, including cancer pain, phantom limb pain, migraine, and cluster headache, looks very promising. Furthermore, psychedelics appear to be generally safe when administered under the careful supervision of trained therapists and medical professionals, and they do not appear to lead to dependence of any kind.
That said, there have been no truly reliable outcomes yet due to the absence of randomized placebo-controlled trials on the clinical efficacy of psychedelics for chronic pain. As a consequence, what appear to be profoundly positive results would perhaps best be interpreted with a grain of salt. It would be a mistake at this early stage to assume that psychedelics are going to be a panacea for chronic pain in its various manifestations, simply because clinical research needs to be done.
Psychedelic self-medication has become increasingly popular, reportedly amounting to approximately 15% of self-reported psychedelic substance use. Considering the widely reported analgesic power of psychedelics, and with over 20% of the population currently suffering from chronic pain, it is perhaps safe to presume the number of people self-medicating with psychedelics to relieve pain is substantial.
Chronic pain is so severe, and conventional medications so ineffective for most, that a significant number of patients are ready and willing to do anything to find relief, including breaking the law and having metal inserted inside their body for at most 50% pain relief.
Psychedelic substances have proven to be incredibly powerful tools in the treatment of mental health conditions, and if the profundity of that therapeutic potential can be translated into pain medicine, patients may be able to alleviate their suffering without having to undergo intense, invasive surgery, or without having electrodes inserted into their spinal cord.
It is very early days, but psychedelics could mean radical improvements for the more than hundreds of millions of chronic pain sufferers around the world.

Comments